According to the CDC, cancer currently ranks as the second leading cause of death in the United States. While heart disease remains the top cause, the difference between heart disease and cancer is surprisingly narrow – about 90,000 lives.
With approximately 1.9 million expected new cases of cancer to be diagnosed this year and roughly 600,000 expected deaths, it begs the question: How long will it take before cancer becomes the number one leading cause of death?
The American Cancer Society provides a sobering perspective on the lifetime risk of developing or dying from cancer. For men, the lifetime risk stands at a staggering 50%, meaning that 1 out of every 2 men in the US will face a cancer diagnosis. Similarly, for women, the lifetime risk is 33%, equating to 1 out of every 3 women being confronted with cancer.
Despite billions of dollars invested in cancer treatment and research, the improvement in mortality rates has been relatively low, ranging between 2-3%. One of the primary reasons for this stagnation is that current care provided does not adequately consider the variations in lifestyle factors, such as nutrition or exercise, or the impact of genes and environmental toxins. Additionally, traditional treatment options often lack the specificity needed to address individualized health needs and goals.
What can we do in the face of this looming cancer crisis? As nurses, we understand the importance of a systematic approach to solving any clinical problem effectively. It’s imperative that we first assess the situation, then implement strategies, and finally, evaluate the outcomes to ensure the effectiveness of our interventions. As a society, we’re often quick to skip the assessment phase, rush straight into intervention and forget to monitor our progress to actually see if the intervention worked.
So, let’s take a step back and check our baseline first. Here are two key areas where individuals can assess and improve their baseline health:
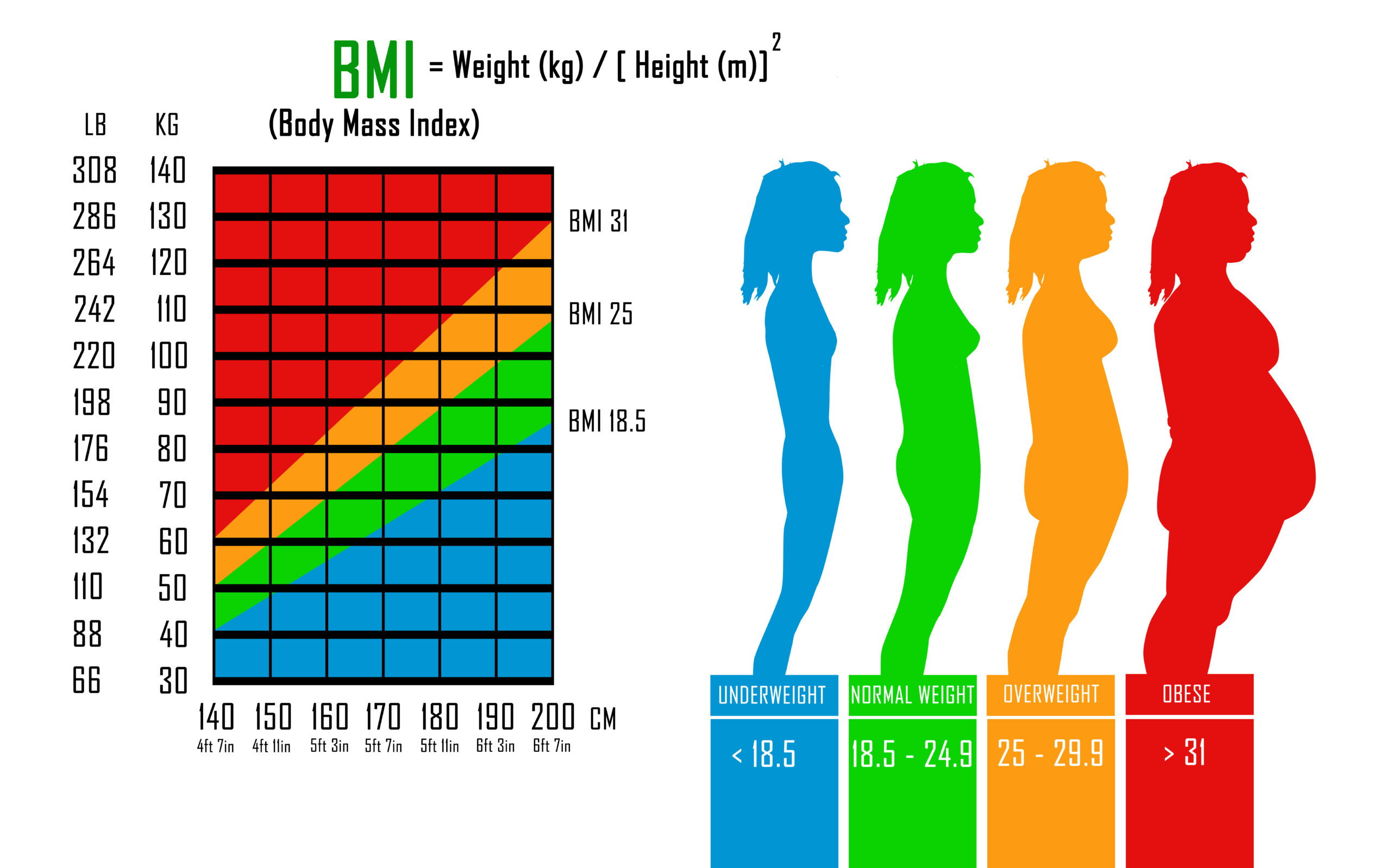
- What is your baseline BMI (Body Mass Index)? Understanding your BMI can help you gauge if you’re at a healthy weight for your height. It’s a simple, but crucial metric for assessing your risk of various health conditions, including obesity and cancer.
- Baseline alcohol intake: Alcohol consumption is a known risk factor for certain types of cancer. It’s essential to assess your alcohol intake honestly.
- In a typical week, how many days do you drink?
- How many drinks do you have each day?
- How many ounces are in each serving of a drink?
- What are the most common types of drinks you consume when you drink?
Staying informed about cancer-related resources and support groups can be immensely beneficial:
- Sober Mom Squad: If you’re a mother looking to reduce or quit alcohol consumption, groups like this can provide a supportive community to help you achieve your goals.
- Read our TCT blog post for helpful ways to offset the negative effects of drinking if you’re trying to cut down.
- There are several, recent books being published about sobriety, indicating that you are not alone in struggling with societal reliance on alcohol. Check out this list to find one that sounds interesting to you.
As we confront the alarming rise of cancer as a leading cause of death, taking proactive steps to assess and improve our baseline health, particularly in terms of BMI and alcohol intake, can make a significant difference. Additionally, staying informed about the latest developments in cancer research and seeking support from relevant groups can contribute to the ongoing fight against this preventable disease.
Wishing you the best on your journey! Stay connected with us by subscribing to our newsletter and following us on Facebook, Instagram or LinkedIn.
Thank you for being part of our community where we share a passion for aging gracefully and saving lives through cancer navigation. #Let’sNavigateCancerTogether